[환자 ‘표류’ 해법, 해외에서 찾다]〈1〉 How did you deal with the shortage of doctors?
獨 “Emergency focus, general surgery is delayed”
Japan predicts shortage of doctors in 20 years and increases numbers
Medical community calls for expansion “still insufficient”
Emergency room at Asclepius Hospital in Hamburg, Germany, on the morning of the 19th of last month. When a male patient in his 50s who collapsed with symptoms of seizures was brought into an ambulance, four medical staff, including an emergency medicine specialist, rushed to the entrance. The medical staff administered first aid in a coordinated manner and sent the patient to the hospitalization ward in just 5 minutes.
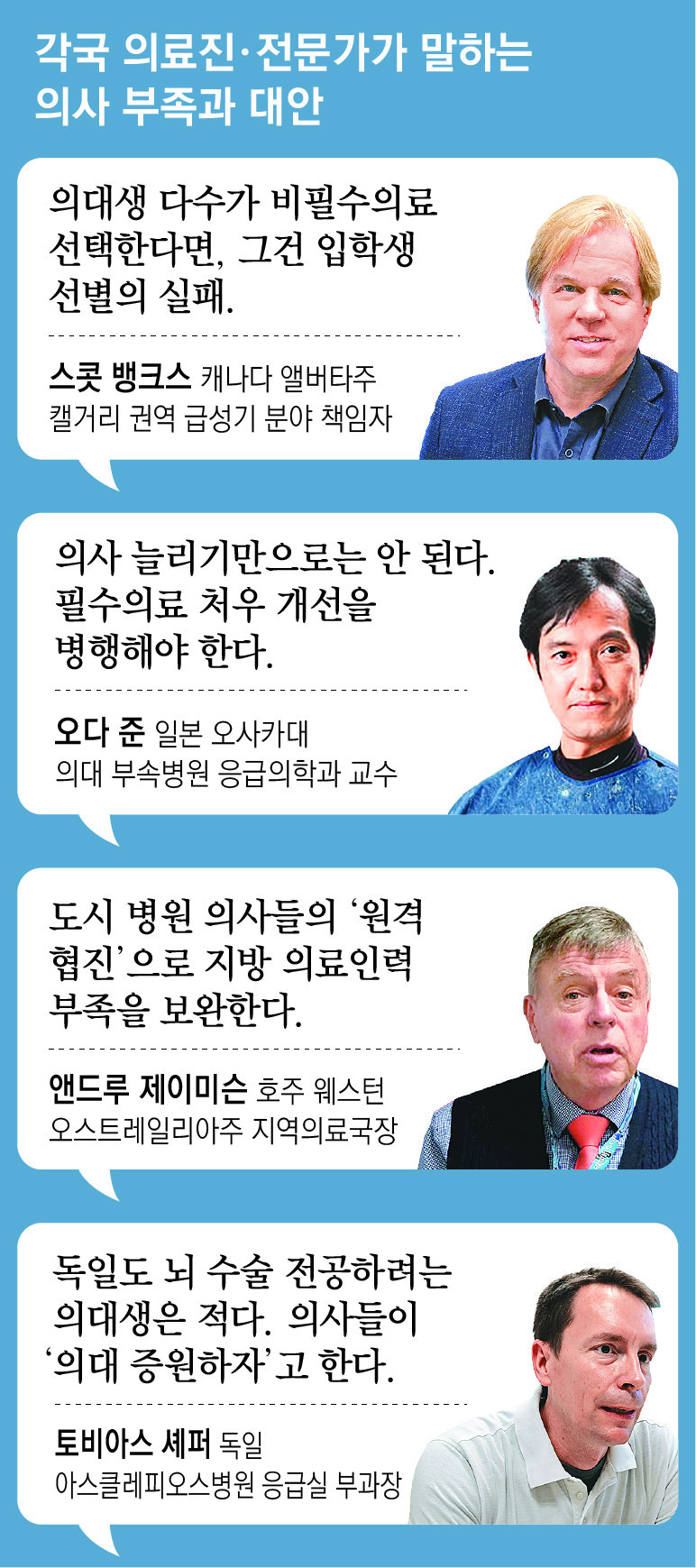
Even overseas, arduous and dangerous essential medical care is a field that doctors avoid. However, in Germany, where the reporter visited, it was not possible to see ‘drifting’ emergency patients wandering around looking for hospitals to receive treatment. Tobias Schaefer, deputy director of the emergency department, said, “Our hospital mainly accepts the most critically ill patients from the surrounding area, but we have rarely been unable to accept seriously ill patients due to lack of staff.” “That doesn’t happen anywhere in Germany,” he said.
Germany, which experienced an aging population before Korea, is benefiting from early expansion of medical school enrollment. As of 2021, there are 4.5 clinical doctors per 1,000 people in Germany, which is 1.7 times the number in Korea (2.6). It is the third largest among member countries of the Organization for Economic Co-operation and Development (OECD). Nevertheless, the German Medical Association still calls on the government to ‘increase the number of medical school students.’ As doctors’ working hours have shortened, their actual medical treatment capacity has actually decreased, and as priority has been given to treating serious emergency patients, waiting times for minor surgeries, etc., are getting longer. “I think Germans still need more doctors,” said Daniel Rörmann, a member of the Güterslosh health advisory board.
The situation is similar in Japan. The Japanese government predicted in 2006 that the doctor shortage would worsen around 2030. Afterwards, the number of medical school students increased from 7,625 in 2007 to 9,420 in 2019. However, essential medical doctors are demanding further expansion, saying, “The number of doctors per bed is still insufficient.”
On the 13th of last month, Professor Jun Oda of the Department of Emergency Medicine, who met at the Advanced Emergency Rescue Center of the Osaka University Medical School Affiliated Hospital in Japan, said, “The number of doctors has increased, but the problem of shortage of manpower in essential medical fields still remains. He said, “We cannot just increase the number of doctors, but we must also take measures to save essential medical care.”
The Dong-A Ilbo reporting team visited 15 sites, including hospitals and emergency services, in five countries, including Japan, Germany, Canada, Australia, and the United States, from August to October this year to find a solution to the domestic essential medical problem of ‘drifting’ of seriously ill and emergency patients. visited. In the process, 44 local experts were interviewed. Overseas, they were struggling to save patients by expanding the number of doctors in advance and developing a system that connects seriously ill and emergency patients with doctors in real time.
On the 19th, President Yoon Seok-yeol announced the ‘Essential Medical Innovation Strategy’ to expand the number of medical school admissions and increase the medical treatment capacity of local national university hospitals. What should we do to avoid repeating the failure of previous governments to reform health care, which resulted in even greater side effects through hasty implementation? Doctors and policy officials met at medical sites in each country said, “What is important is the will to implement and detailed design.”
獨Essential medical staff receive greater compensation than private doctors
Increasing avoidance of arduous surgery by Japanese and Korean surgeons
“It is difficult to solve the problem by simply expanding the number of medical school students.”
On the 19th, the government made clear its intention to increase the number of medical school admissions starting from the 2025 school year. However, the real challenge is to create an environment where the increased number of doctors can work in local and essential medical fields. If these people flock to Seoul or leave the skin care field, the ‘drift’ of severe emergency patients may not be resolved, but national medical expenses may only increase. In countries such as Germany, Japan, and Canada that the reporting team visited, there was various policy support to attract doctors to essential medical services.
Germany sets a limit on the number of private hospitals that can be opened in a given region for each treatment subject through the ‘capacity system for private hospitals’. This is a measure to prevent a shortage of essential doctors at large hospitals due to a reckless rush to open clinics. In fact, Germany has 1.47 surgical specialists per 1,000 people, which is more than twice that of Korea (0.71). On the 19th of last month, Mona Lindschau, a pediatrician at Eppendorf Hospital in Hamburg, said, “Specialists in essential medical fields at large hospitals usually receive more compensation than private practitioners, so private practice permits are not selling well.” On the other hand, in Korea, the income is much better if you open a local clinic and perform skin care treatments or physical therapy. This is one of the reasons why there is a shortage of surgeons.
Despite these policies, doctors’ avoidance of essential medical care is said to be gradually spreading in Germany. This is because ‘work-life balance’ is an important topic. Tobias Schaeffer, deputy director of Asclepius Hospital, said, “In particular, young doctors are reluctant to become neurosurgeons who perform brain surgery because the work is hard and they are often on call.” Accordingly, the government is attracting shortage of surgical doctors from overseas. Han Seong-guk, a Korean-German nephrologist, said, “We are running separate professional language tests and qualification tests for immigrant doctors.”
 On the 12th of last month, Professor Kentaro Kazino, Department of Emergency Medicine, Kansai University Medical School Hospital, Japan, is inspecting first aid equipment in an emergency patient transport vehicle (doctor car). Since around 2006, Japan has been making efforts to solve essential medical issues by expanding the number of medical school students and introducing a mandatory regional work system. Osaka =
On the 12th of last month, Professor Kentaro Kazino, Department of Emergency Medicine, Kansai University Medical School Hospital, Japan, is inspecting first aid equipment in an emergency patient transport vehicle (doctor car). Since around 2006, Japan has been making efforts to solve essential medical issues by expanding the number of medical school students and introducing a mandatory regional work system. Osaka = Japan significantly expanded the number of medical school students and introduced the ‘Local Medical Securing Scholarship’. It is a system that selects some of the medical school seats through a separate selection process and provides scholarships, but requires students to work in areas where hospitals and clinics are lacking, usually for about 10 years. This is similar to the ‘regional doctor system’ that the Moon Jae-in administration announced in July 2020 but shelved in the face of strong opposition from the medical community.
In 2007, the first year of the system’s introduction, there were 183 medical students receiving scholarships to secure local medical care, accounting for only 2.4% of all medical students. However, in 2020, the number increased significantly to 1,679 (18.2% of the total). The number of doctors in rural areas, which had been rapidly decreasing, has also rebounded since 2010, increasing by 12.1% in 2018 compared to eight years ago.
However, local experts pointed out that although this system may have helped put out the urgent fire of ‘local medical collapse’, it did not solve the problem of avoidance of essential medical subjects. Hideharu Tanaka, professor of emergency medicine at Kokushikan University Medical School in Tokyo, said, “While dermatology and plastic surgery are very popular in Japan, emergency medicine, obstetrics and gynecology, etc. are ‘4K’ (Japanese short for ‘difficult, dirty, dangerous, unfashionable’). ) He said, “Doctors avoid it because it is considered a profession,” and added, “It is a difficult problem to solve unless we increase the treatment of essential medical fields.”
This suggests that the ‘trickle-down effect’ of expanding medical school seats alone cannot completely resolve essential medical issues. We must improve working conditions in the essential medical field and ensure that emergency patients receive treatment first. Australia is actively utilizing information and communication technology (ICT). Andrew Jamieson, Regional Medical Director of Western Australia, said, “We, too, have doctors reluctant to work in small towns. Instead, skilled doctors from large hospitals are supplementing the shortage of local medical personnel through ‘remote collaborative care.’”
It is pointed out that the Canadian case, which conducts personality evaluations such as reasons for wanting to become a doctor and volunteer experience in addition to grades when entering medical school, is also worthy of reference. Scott Banks, director of the acute care division in the Calgary, Alberta, Canada area, said, “Doctors in the dermatology field make better money in Canada, but this does not mean that the essential medical field is experiencing a manpower shortage.” “If you choose the medical field, it is a failure in screening medical school students,” he said.
※ This article was supported by the Press Promotion Fund raised through government advertising fees.
| Special reporting team |
| ▽ ▽Reporters Ji-woon Lee, So-young Kim, and Moon-soo Lee (Ministry of Policy and Society) |
Osaka, Hamburg, Calgary, Perth, Boston = Special Reporting Team
Source: Donga
Mark Jones is a world traveler and journalist for News Rebeat. With a curious mind and a love of adventure, Mark brings a unique perspective to the latest global events and provides in-depth and thought-provoking coverage of the world at large.